TrumpRx: The White House's Bold Play to Cut Weight Loss Drug Costs — But Will It Really Help Americans?
President Trump announces deals with Eli Lilly and Novo Nordisk to slash obesity drug prices through controversial direct-to-consumer platform, but skeptics question who actually benefits
In the Oval Office on Thursday morning, President Donald Trump stood beside pharmaceutical executives and announced what he called a "groundbreaking" deal to make weight loss drugs affordable for millions of Americans. The agreement with Eli Lilly and Novo Nordisk promises to cut the costs of blockbuster obesity medications like Wegovy and Zepbound to as low as $149 per month through TrumpRx.gov, a government-run direct-to-consumer pharmaceutical website set to launch in early 2026.
"The United States is done subsidizing the health care of the rest of the world," Trump declared, echoing a familiar refrain from his administration's ongoing battle with pharmaceutical companies. "By taking this bold step, we're ending the era of global price gouging at the expense of American families."
But beneath the political theater and the promise of dramatic savings lies a more complicated reality — one that raises questions about who will actually benefit from this deal, and whether TrumpRx represents genuine reform or clever marketing wrapped in the flag of healthcare populism.
The Deal: What Americans Are Actually Getting
According to the agreement announced Thursday, the lowest doses of Novo Nordisk's Wegovy will cost $149 per month through TrumpRx, while Eli Lilly's Zepbound will start at $299 — a significant drop from current list prices that exceed $1,000 monthly. The deals also expand Medicare and Medicaid coverage for obesity drugs, though the precise eligibility criteria remain unclear.
For patients who might eventually access oral versions of these medications, pending FDA approval, the starting dose would be priced at $145 per month. Health and Human Services Secretary Robert F. Kennedy Jr. described the negotiations as taking "months and months" to complete, while Trump added, "You think it was easy dealing with these people? It wasn't."
The pharmaceutical companies have also committed to investing billions in U.S. manufacturing — $27 billion from Eli Lilly and $10 billion from Novo Nordisk — and to offering their drugs at "most-favored-nation" pricing, meaning Americans would theoretically pay rates comparable to those in other developed countries.
The Reality Check: Who's Left Behind?

What the White House didn't emphasize in Thursday's announcement is perhaps more telling than what it did. TrumpRx won't actually sell or distribute medications. Instead, it will function as a referral service, redirecting consumers to manufacturers' direct-to-consumer channels. For the 92% of Americans with health insurance, industry analysts suggest these cash prices may still be higher than what their insurance plans already cover.
"The biggest question is this: Will patients be able to afford these drugs by paying out of pocket without having insurance help, and also by not having those payments count toward their deductibles?"
— Dr. Mariana P. Socal, Johns Hopkins Bloomberg School of Public Health
Dr. Socal's concern cuts to the heart of the matter. For insured patients, paying cash through TrumpRx means those expenses won't count toward annual deductibles or out-of-pocket maximums — potentially costing them more in the long run. The platform appears designed primarily for the uninsured or underinsured, a crucial segment of the population but far from the majority of Americans struggling with obesity.
Even the promised savings may not be as dramatic as they appear. Consider Xeljanz, one of the Pfizer drugs available through an earlier TrumpRx deal. The White House touted a 40% discount, but that still leaves the monthly cost around $3,600 for a drug whose list price exceeds $6,000. As health policy expert Stacie Dusetzina pointedly asked, "How is this a reasonable cash price? It really isn't."
A Pattern Emerges: Politics Before Patients?
The TrumpRx initiative didn't emerge in a vacuum. It follows the Trump administration's decision to scrap a Biden-era proposal that would have let Medicare and Medicaid cover GLP-1 drugs for treating obesity. Now, months later, the administration is pursuing a different path — one that bears the president's name and allows him to claim credit for negotiating deals directly with pharmaceutical companies.
The timing is also strategic. Thursday's announcement came just one day after Trump's self-imposed deadline for drugmakers to comply with his "Most Favored Nation" executive order — and conveniently ahead of his threatened 100% tariff on brand-name pharmaceutical imports. Companies that strike deals with the administration, like Pfizer, Eli Lilly, and Novo Nordisk, receive three-year tariff exemptions.
It's a masterclass in leveraging executive power, but the question remains whether this approach actually serves patients better than comprehensive Medicare and Medicaid coverage reforms would have. Political analysts like Dave Wasserman have long documented how healthcare policy becomes a battleground for competing visions of government's role — and TrumpRx exemplifies this tension perfectly.
The Industry Perspective: Carrots and Sticks
For pharmaceutical companies, the TrumpRx deals offer both opportunity and constraint. They gain access to a government-backed platform and tariff relief, but they also commit to pricing structures that may limit future flexibility. The drug industry has warned that "importing foreign price controls would undermine American leadership, hurting patients and workers," according to PhRMA senior vice president Alex Schriver.
Yet the companies are playing along — at least for now. Novo Nordisk's Doug Doustdar noted that cash-pay options for Ozempic and Wegovy are "the channel that's right now growing the most," suggesting that direct-to-consumer sales represent a growing market segment that companies are eager to capture, even at reduced margins.
The landscape bears similarities to other high-stakes Washington negotiations. Capitol Hill veterans like Jake Sherman have documented how legislative deals often satisfy political needs while leaving substantive policy questions unresolved. TrumpRx may be following a similar playbook.
The Unanswered Questions
Journalists and health policy experts have identified numerous gaps in the TrumpRx rollout. When exactly will the website launch? Which specific drugs will be available at launch versus later? How will the platform compare to existing discount services like GoodRx or Mark Cuban's Cost Plus Drug Company? Will the promised "most-favored-nation" prices actually represent the lowest available rates, or just the lowest prices pharmaceutical companies claim to offer abroad?

Most critically, will TrumpRx actually lower costs for Americans who already have insurance, or will it primarily serve as a government-sponsored alternative for a smaller subset of the population?
The Human Element: Beyond Politics and Pricing
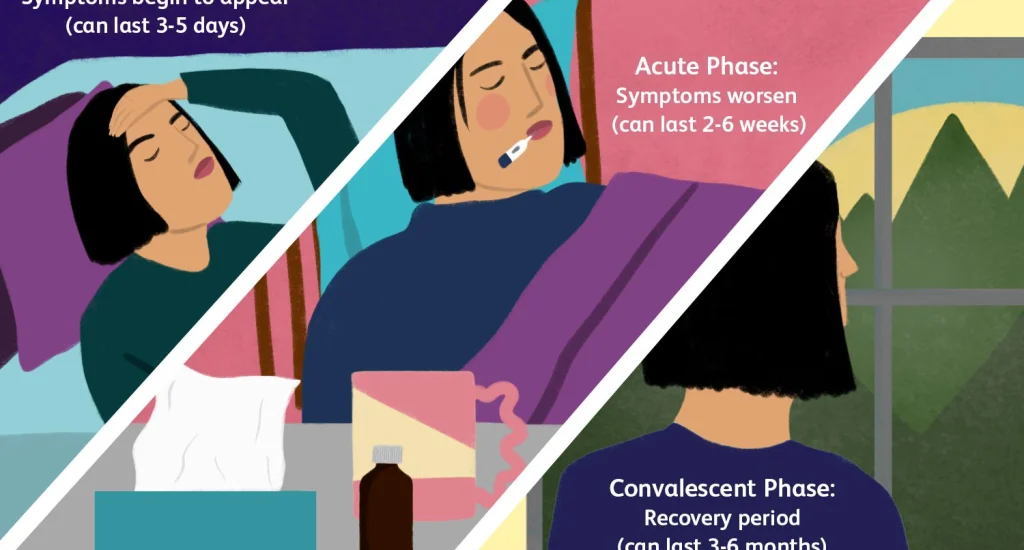
Lost in the political positioning and pricing debates are the real people affected by obesity — roughly 40% of Americans, according to CDC data. These are individuals dealing with a chronic disease that increases their risk of heart disease, diabetes, stroke, and premature death. For them, GLP-1 medications represent not just weight loss but potentially life-saving treatment.
The desperation is palpable. Patients have been scrambling to access these drugs through various channels, driving demand so high that supply constraints have become routine. Just as bettors were left stranded when FanDuel crashed during peak NFL Sunday, patients are often left waiting when popular obesity drugs run out of stock. Costco recently began offering Wegovy and Ozempic at $499 for uninsured patients — a discount, certainly, but still prohibitively expensive for many Americans.
"This is not about losing weight — this is about making America healthy again," a senior administration official told reporters. "This is about preventing strokes, this is about preventing end-stage renal disease."
The sentiment is noble, but whether TrumpRx can deliver on that promise remains to be seen. Much like how Jayden Daniels' injury cast uncertainty over the Commanders' season, the long-term impact of TrumpRx on America's healthcare system remains uncertain until we see how it functions in practice.
A Cynical Compromise or Genuine Progress?
As with most healthcare policy, the truth about TrumpRx likely falls somewhere between the administration's triumphant claims and critics' dismissive skepticism. Yes, some Americans — particularly the uninsured — may benefit from lower cash prices for obesity drugs and other medications. The expanded Medicare and Medicaid coverage could help vulnerable populations access life-changing treatments.
But the platform's limitations are equally real. By focusing on direct-to-consumer sales rather than comprehensive insurance reform, TrumpRx risks creating a two-tiered system where the insured pay through traditional channels while the uninsured navigate a government website that doesn't actually sell drugs, just points them to manufacturers.
"The administration is framing this as a cost-saving strategy, because you are not adding margins for insurers or PBMs. But the biggest question is this: Will patients be able to afford these drugs by paying out of pocket without having insurance help?"
That question, posed by Dr. Socal, deserves an answer before we declare TrumpRx a healthcare revolution. Until the website launches, until we see actual patient outcomes, until we understand who saves money and who doesn't, we're left with promises and press conferences — and the nagging suspicion that genuine healthcare reform requires more than a website bearing a president's name.
What Comes Next
The Trump administration promises TrumpRx will be operational by early 2026, possibly as soon as January. Additional pharmaceutical companies are reportedly in negotiations to join the platform. For political observers like Eric Daugherty, these developments represent another chapter in the ongoing struggle to reconcile free-market healthcare with government intervention.
Meanwhile, millions of Americans with obesity will continue weighing their options — literally and figuratively. They'll calculate whether $149 for Wegovy or $299 for Zepbound represents affordable care or just another unattainable promise. They'll wonder if their insurance might cover these drugs at lower out-of-pocket costs. They'll ask their doctors, scroll through Reddit forums, and make difficult decisions about their health and their wallets.
And when TrumpRx finally launches, we'll all learn whether this bold experiment in government-negotiated drug pricing delivers on its promise or becomes another cautionary tale of politics over policy, branding over substance.
For now, the only certainty is this: America's healthcare crisis won't be solved by a website alone, no matter whose name is on it.
Related Articles