Is a Viral Rash Contagious? What You Need to Know in 2025
Separating medical fact from fear — understanding viral rashes, transmission risks, and when that suspicious skin condition actually puts others at risk
You notice red bumps spreading across your child's torso. Or perhaps you wake up with an itchy rash crawling up your arms. The internet search that follows is almost always the same: "Is this contagious?" Because in our hyperconnected world, where we live in close quarters and share spaces constantly, that question matters as much as what the rash actually is.
The term "viral rash" itself causes confusion. Does "viral" mean it spreads like wildfire through classrooms and offices? Does it mean you should quarantine immediately? Or is it simply describing the underlying cause — a virus — without implications about person-to-person transmission?
In November 2025, as respiratory viruses circulate seasonally and new variants occasionally emerge, understanding which rashes pose contagion risks and which don't has become essential knowledge for parents, teachers, healthcare workers, and anyone navigating shared spaces. The answer, frustratingly, is: it depends entirely on which virus is causing the rash.
Understanding Viral Rashes: The Basics
A viral rash is simply a skin reaction triggered by a viral infection. According to the Centers for Disease Control and Prevention, dozens of different viruses can cause characteristic rashes, each with different contagion profiles, transmission methods, and public health implications.
The critical distinction that many people miss: whether a rash itself is contagious is separate from whether the underlying virus is contagious. In most cases, you cannot catch a rash by touching someone who has one. But you might catch the virus that caused their rash, which could then cause a rash in you — though it might also cause entirely different symptoms, or no symptoms at all.
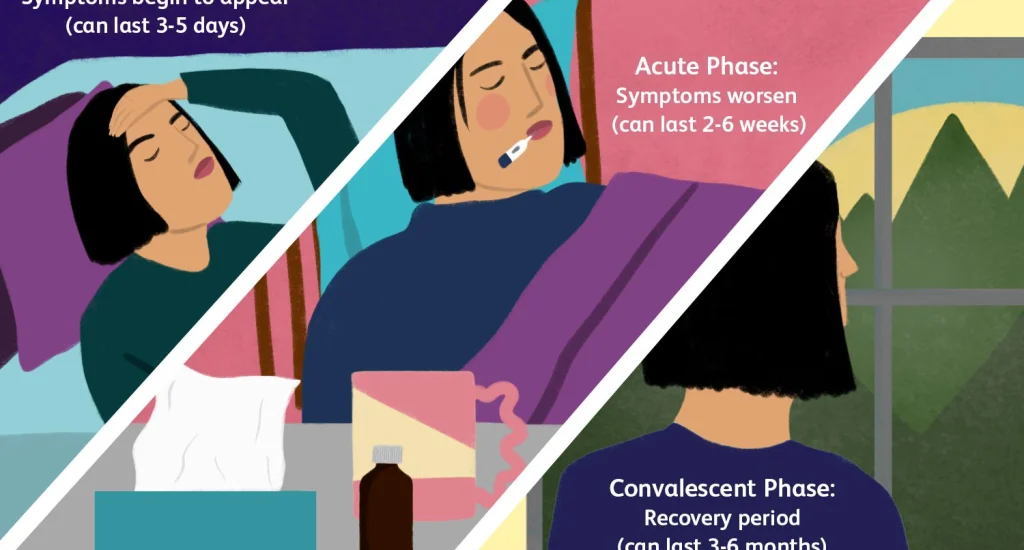
This nuance matters enormously for practical decisions about school attendance, workplace policies, and social interactions. A person with a viral rash might be highly contagious, minimally contagious, or not contagious at all, depending on which virus caused it and what stage of infection they're in.
"The question isn't really 'is the rash contagious' — it's 'is the person with the rash shedding virus that can infect others.' Those are fundamentally different questions with different answers."
— Infectious disease specialist quoted by Mayo Clinic
Common Viral Rashes: The Contagion Spectrum
Not all viral rashes pose equal transmission risks. Here's what current medical evidence tells us about the most common viral rashes and their contagion profiles:
Highly Contagious Viral Rashes
Chickenpox (Varicella): Extremely contagious from 1-2 days before the rash appears until all blisters have crusted over. The virus spreads through respiratory droplets and direct contact with fluid from the blisters. According to the CDC, chickenpox has a secondary attack rate of approximately 90% in susceptible household contacts — meaning if one family member gets it, nearly everyone without immunity will too.
Measles: Among the most contagious diseases known to medicine. A person with measles can infect up to 90% of non-immune people in close contact. The distinctive red, blotchy rash typically appears 3-5 days after symptoms begin, but the person has been contagious since before the rash emerged. Airborne transmission makes measles particularly dangerous in shared spaces.
Hand, Foot, and Mouth Disease: Common in children, caused by enteroviruses like coxsackievirus. Highly contagious through respiratory secretions, fecal matter, and direct contact with blister fluid. People remain contagious throughout the illness and sometimes for weeks after symptoms resolve, even though they feel fine.
Moderately Contagious Viral Rashes
Fifth Disease (Erythema Infectiosum): Caused by parvovirus B19, produces a distinctive "slapped cheek" appearance in children. The paradox of fifth disease: by the time the rash appears, the person is usually no longer contagious. They were most infectious during the week before the rash emerged, when they just seemed to have a mild cold.
Roseola: Common in infants and toddlers, caused by human herpesvirus 6. Contagious during the fever phase before the rash appears. Once the characteristic pink rash emerges as fever breaks, the child is typically no longer spreading virus.
Minimally or Non-Contagious Viral Rashes
Viral exanthem: A general term for rashes caused by various common viruses. Many of these pose minimal transmission risk by the time the rash is visible, though the underlying respiratory or gastrointestinal virus might still be transmissible through other routes.
Shingles (Herpes Zoster): Caused by reactivation of dormant chickenpox virus. A person with shingles can transmit varicella-zoster virus to someone who's never had chickenpox, causing chickenpox in that person rather than shingles. However, transmission requires direct contact with fluid from the rash blisters, not casual contact or airborne spread.
The Transmission Question: How Viral Rashes Actually Spread
Understanding transmission mechanisms helps clarify risk. Viral rashes don't jump from person to person through mystical means — they follow specific biological pathways that determine actual contagion danger.
Respiratory droplet transmission: Many viruses that cause rashes spread primarily through coughs, sneezes, and talking. The rash itself is irrelevant to transmission — it's the respiratory viral shedding that matters. This is why someone with fifth disease is contagious before the rash appears but not after.
Direct contact transmission: Some viral rashes involve fluid-filled blisters containing infectious virus. Chickenpox and shingles fall into this category. Touching the blisters or items contaminated with blister fluid can transmit virus. Once blisters crust over, this transmission route closes.
Fecal-oral transmission: Enteroviruses causing hand, foot, and mouth disease can spread through contaminated surfaces, particularly in childcare settings where diaper changing and hand hygiene challenges are constant. The virus can persist in stool for weeks after symptoms resolve.
Airborne transmission: Measles and varicella-zoster can remain suspended in air for extended periods, capable of infecting people who enter a room hours after an infectious person left. This makes these viruses particularly dangerous and explains why they require more stringent isolation precautions.
Current Viral Rash Patterns

Public health surveillance in late 2025 shows seasonal patterns that parents and healthcare providers have come to expect. According to recent data from the World Health Organization, enterovirus activity typically peaks in late summer and fall, making hand, foot, and mouth disease more common during these months. Measles outbreaks continue occurring in communities with low vaccination rates, creating periodic public health emergencies.
The COVID-19 pandemic permanently changed how we think about contagious illness and shared spaces. That heightened awareness now extends to all communicable diseases, including those causing rashes. Schools and childcare facilities have updated policies about when children with rashes can return, generally requiring medical clearance that confirms either non-contagious status or appropriate treatment.
When to Worry: Red Flags Beyond Contagion
While contagion concerns dominate parental anxiety about rashes, other factors sometimes matter more. Certain viral rashes signal potentially serious conditions requiring immediate medical attention:
- Rash accompanied by high fever and severe headache: Could indicate meningitis or encephalitis
- Rash that doesn't blanch when pressed: Might suggest serious bacterial infection like meningococcemia
- Rash with difficulty breathing or swelling: Could represent severe allergic reaction requiring emergency care
- Rash in immunocompromised individuals: Even typically mild viral infections can become dangerous
- Rash in pregnant women: Some viral infections like rubella and parvovirus B19 pose risks to fetal development
The contagion question, while important, shouldn't overshadow these more urgent medical concerns. A non-contagious rash can still represent serious illness requiring immediate treatment, while a highly contagious rash might be medically benign even as it spreads through communities.
"We always tell parents: worry about your child's clinical condition first, contagion second. A very sick child with a non-contagious rash needs more urgent attention than a mildly ill child with something highly transmissible."
— Pediatrician quoted in medical journal interview
Practical Guidance: What to Do When Rashes Appear
When you or your child develops a rash that might be viral, several practical steps help protect both the affected person and the community:
Seek medical evaluation: Don't rely on internet diagnosis for rashes. Many conditions produce similar appearances but have vastly different implications. A healthcare provider can usually identify the cause and provide guidance about contagion period, treatment needs, and return-to-school or work timelines.
Practice isolation during uncertain periods: If you don't yet know what's causing a rash, err on the side of caution and avoid close contact with vulnerable individuals — infants, pregnant women, immunocompromised people — until medical evaluation clarifies the situation.
Maintain hygiene measures: Frequent handwashing, covering coughs and sneezes, and avoiding sharing personal items remain effective across most viral transmission routes. These basic measures reduce spread even when you're unsure about specific contagion mechanisms.
Follow exclusion guidelines: Schools and childcare facilities typically have policies about when children with various illnesses can return. These policies balance public health protection with recognition that excluding children for every minor illness isn't practical or beneficial.
Communicate with contacts: If you or your child is diagnosed with a contagious viral rash, notify close contacts so they can watch for symptoms and consult healthcare providers if needed. This is particularly important for measles, chickenpox, and other highly transmissible infections.
The Vaccination Factor
Several viral rashes that once caused widespread concern are now largely preventable through vaccination. The measles-mumps-rubella (MMR) vaccine has dramatically reduced measles and rubella incidence in vaccinated populations. The varicella vaccine has made chickenpox increasingly rare among vaccinated children, though breakthrough infections can still occur.
Vaccination status fundamentally changes the viral rash landscape. In communities with high vaccination coverage, highly contagious viral rashes become rare, reducing overall transmission risk. In communities with low vaccination rates, outbreaks occur periodically, creating situations where contagion concerns become urgent public health matters rather than individual medical questions.
The Bottom Line on Viral Rash Contagion
So, is a viral rash contagious? The honest answer remains: it depends. Some viral rashes occur during highly contagious phases of illness. Others appear precisely when the person is no longer infectious. Some require direct contact with rash fluid to transmit. Others spread through respiratory droplets having nothing to do with the rash itself.
What matters more than memorizing which rashes are contagious is understanding the principles: viral rashes indicate viral infections, those infections have varying transmission routes and timelines, and medical evaluation provides the specific guidance needed for individual situations.
In November 2025, as we navigate another season of circulating viruses, the questions parents ask haven't changed much from generations past. What has changed is our scientific understanding of viral transmission, our public health infrastructure for monitoring and responding to outbreaks, and our collective awareness — heightened by recent pandemic experience — that individual health decisions affect community wellbeing.
The child with a suspicious rash isn't just a medical problem to solve. They're a node in a transmission network that connects families, schools, and communities. Understanding whether that rash signals contagion risk helps everyone make informed decisions that balance individual needs with collective protection.
And sometimes, the most responsible action is the simplest: when in doubt, call your doctor. Because while the internet can provide general information about viral rashes and contagion, only medical evaluation of your specific situation can provide the guidance that actually matters — not whether viral rashes in general can be contagious, but whether this rash, on this person, at this moment, poses risks that require specific precautions.
That's not uncertainty masquerading as wisdom. It's recognition that medicine remains fundamentally individual even when we discuss population-level patterns. The viral rash question, like so many health questions, resists simple universal answers because biology is complicated, viruses are diverse, and every patient's situation includes unique factors that no general article can fully address.
But armed with better understanding of how viral rashes work and spread, you're better equipped to ask the right questions when those red bumps appear — and to understand the answers when medical professionals provide them.
Related Articles